Physician Assistant Heals Broken Hearts
Cardiac care specialist discusses the latest minimally invasive procedures that have a huge impact on heart health.
Lesley Field’s path into cardiology began when she developed arrhythmias as an elite level triathlete. During the investigation into her heart problems with cardiologists and electrophysiologists, Field left with a healed heart and a passion for a career in cardiac health.
“Cardiology really touches on so many different areas of the body that it really forces you to stay on top of much of your medical knowledge, which I enjoy,” says Field, a physician assistant (PA) who received her degree from Touro University California.
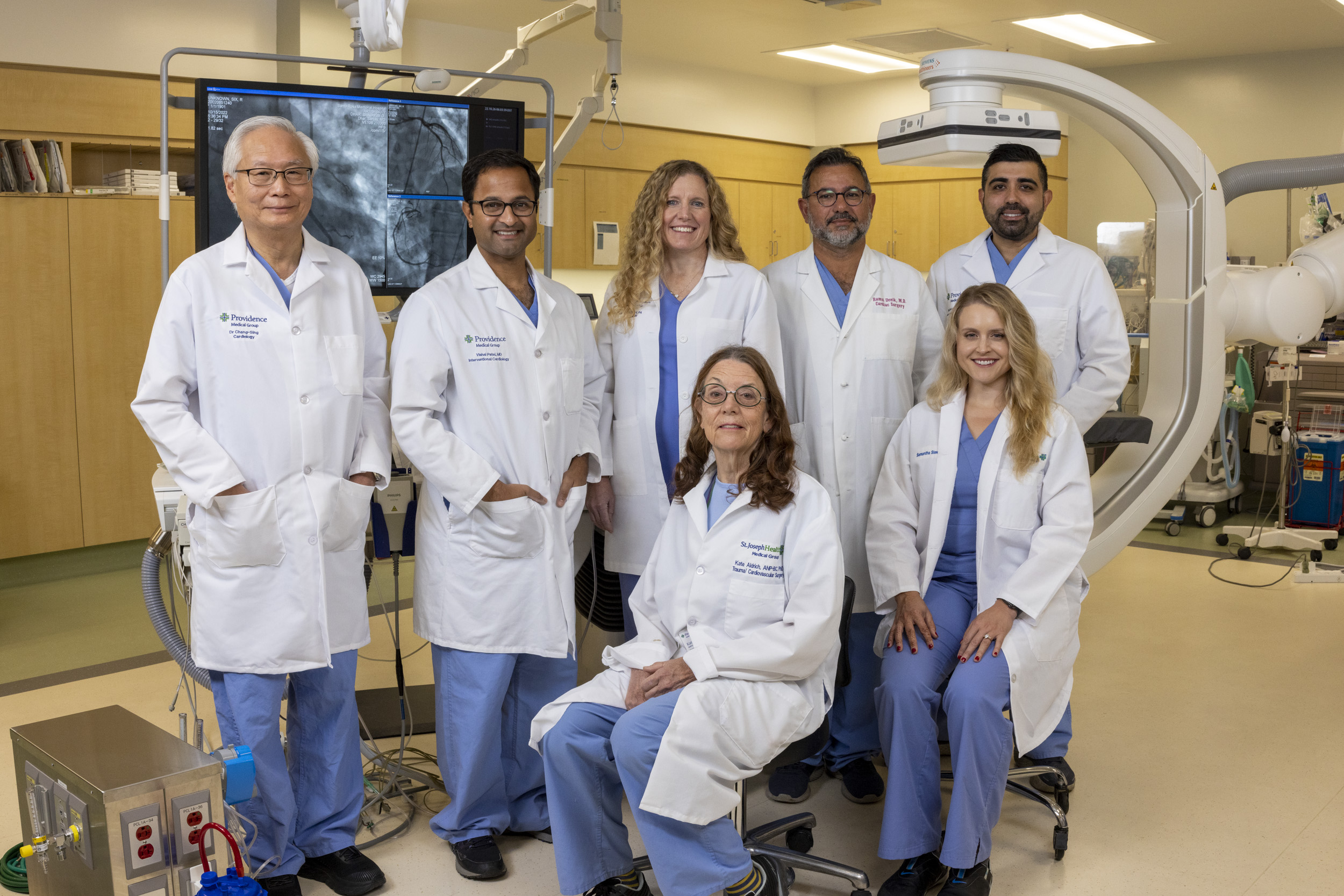
In her current role as a PA on the structural heart team at Providence Santa Rosa Memorial Hospital, Field works in interventional cardiology, a specialty that diagnoses and provides minimally invasive procedures for patients with heart conditions. By utilizing advanced imaging technology to efficiently assess patients’ needs, they perform cardiac repairs without opening the chest. Here are three procedures that Field and her team use to mend broken hearts:
- Aortic stenosis is a condition caused by a narrowed aortic valve, forcing the heart to work harder, and causing fatigue and chest pain. Transcatheter Aortic Valve Replacement (TAVR) is a minimally invasive procedure where a bioprosthetic valve is delivered through a catheter into the heart. This new valve is expanded inside the existing defective valve, improving life expectancy with low risks of complications. Without surgery or TAVR, patients with severe aortic stenosis have a high risk of death within one year of diagnosis.1 The TAVR device functions like a healthy valve with 90% survival at five years, and a low risk of death, stroke, or hospitalization.2
- The MitraClipTM, developed by Abbott, treats severe mitral regurgitation (leaky heart valve). Before its introduction, open heart surgery was often the only option for patients with symptoms like shortness of breath, fatigue, cough, fainting, and difficulty exercising caused by the condition. The MitraClipTM is delivered through a catheter into the heart, where a small clip is attached to the mitral valve leaflets, restoring normal blood flow. The Global EXPAND study showed the device reduced mitral regurgitation by 89%, and after one year 78% of patients had mild or no symptoms.3
- Previously, those with Atrial Fibrillation (AFib), a condition where the heart’s pumping is irregular, had to take daily blood thinners to prevent blood clots. When a patient can’t take blood thinners due to conditions such as stomach ulcers, bleeding, falls, or head trauma, then invasive surgery is required. The WATCHMAN device addresses this by blocking the opening of the left atrial appendage without heart surgery. By sealing this area, the device prevents clot formation without interfering with heart function or requiring blood thinners.
These minimally invasive procedures help patients with cardiac problems without the risk of surgery. Field says that between the evolutions in cardiology and the individual conditions that patients arrive with, every situation requires a customized solution to address their issues in the best way.
“Patients often have multiple health circumstances like kidney disease, diabetes, high blood pressure, or cancer. It’s a puzzle to figure out what’s the biggest priority and what needs to be resolved first,” says Field, who finds motivation in finding solutions to help patients. “I manage them when they’re in the hospital, resolving any acute issues, and connecting to other specialists. It’s complex, but I’ve discovered that I like the challenge.”
- Graham H Bevan, MD, David A Zidar, MD, Richard A Josephson, MS, MD, and Sadeer G Al-Kindi, MD 2019, Mortality Due to Aortic Stenosis in the United States, 2008-2017. JAMA Jun 11;321 (22): 2236-2238.
- Partner 3 Trial Funded by Edwards Lifesciences; PARTNER 3 ClinicalTrials.gov number, NCT02675114.
- Kar S Core-Lab Adjudicated Contemporary Clinical Outcomes at 1 year with MitraClip TM (NTR/XTR) System from Global EXPAND Study. Data presented at TCT 2020.
